Medication for autoantibodies also effective for Long COVID
World’s first successful treatment attempt of a patient with Long COVID Syndrome at Department of Ophthalmology at Universitätsklinikum Erlangen
As part of an individual treatment attempt and thanks to medication originally developed for treating heart disease, a team of doctors at the Department of Ophthalmology at Universitätsklinikum Erlangen has successfully treated a 59 year old man suffering from Long COVID syndrome so that he is now free of symptoms. Whether the active ingredient BC 007 can also help others affected by the disease is soon to be examined in a clinical study. ‘At the moment we are unable to treat any others with the drug because it has not yet undergone all the relevant trials,’ explains Prof. Dr. Christian Martin, assistant chief physician at the Department of Ophthalmology.
Doctors at the Department of Ophthalmology as well as the Department of Medicine 1– Gastroenterology, Pneumology and Endocrinology (Director: Prof. Dr. Markus F. Neurath) and the Department of Medicine 3 – Rheumatology and Immunology (Director: Prof. Dr. Georg Schett) had already discovered during the reCOVer study that patients who have recovered from Covid-19 still have significantly limited blood flow to the eyes even if several months have passed since the infection. The idea behind the treatment attempt was that the changes to the blood flow are certainly not limited to the eye, but are probably affecting the entire body.
In conjunction with Dr. Gerd Wallukat, who has been collaborating with the team for many years and is a former employee of the Max Delbrück Centre for Molecular Medicine in Berlin, the team of doctors found certain proteins, which they have been studying for several years in the context of glaucoma, in the blood of Covid-19 patients months after the infection: autoantibodies against G protein-coupled receptors (GPCR). ‘This means that the immune response, which is in itself a good thing, starts to attack the body, producing substances that can be harmful. This can have serious consequences,’ explains Dr. Dr. Bettina Hohberger, who is a specialist at the Department of Ophthalmology in Erlangen. If the body produces increasing amounts of antibodies, they may attack different structures in the body. While testing the blood samples, the interdisciplinary team of doctors and scientists discovered that patients have a large number of these proteins after a coronavirus infection. ‘We are familiar with one of these autoantibodies from glaucoma and know that it has a detrimental effect on the flow of blood to the eyes,’ explains Dr. Hohberger.
Her long-term collaboration with Dr. Wallukat meant that she had already heard of a medication that can bind these damaging autoantibodies. This would make it possible to make the autoantibodies harmless and potentially improve the circulatory disorders. The drug underwent pre-approval trials for patients with severe heart disease a few years ago by Dr. Wallukat, his colleague Dr. Annekathrin Haberland, and some former heart surgeons at the German Heart Centre Berlin. ‘I originally hoped to help my glaucoma patients with the drug,’ remembers Dr. Hohberger. ‘When we saw the results generated by the collaboration projects for Long COVID, it was as if several small pieces of a jigsaw puzzle fell into place. It was entirely feasible that the drug could also improve the symptoms of Long COVID.’
Circulation greatly improved
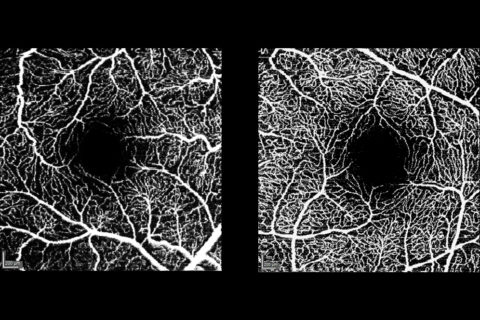
When a patient on the Erlangen glaucoma register who suffers from glaucoma reported his symptoms after recovering from coronavirus – loss of taste, serious problems with concentration and fatigue, which severely restricted him in his professional and private life – the team at the Department of Ophthalmology wanted to offer their assistance. During the treatment with the drug BC 007 developed in Berlin, the 59 year old man received the drug intravenously and remained at Universitätsklinikum Erlangen for three days. ‘His condition improved even after only a few hours. When we discharged him, the patient said he felt his condition had improved considerably and this was confirmed with his autoantibody levels,’ says the team of physicians. His problems with concentration also vanished, his ability to function increased and he regained his sense of taste. ‘Overall, there has been a significant improvement in the blood flow in the capillaries we were able to measure in the eye.’ The team at the Department of Ophthalmology believes that the patient’s symptoms from Long COVID have disappeared due to the improvement in blood flow. Dr. Hohberger was nominated for the 2020 Galenus von Pergamon Award in the fundamental research category for this use of a drug to make autoantibodies harmless in patients with glaucoma.
ReCOVer Study
In conjunction with the intensive care unit at the Department of Medicine 1– Gastroenterology, Pneumology and Endocrinology, which has been treating coronavirus patients since early 2020, and the Department of Medicine 3 – Rheumatology and Immunology, the research team from the Department of Ophthalmology examined the blood flow in the capillaries (the smallest blood vessels) of Covid-19 patients. The scientists used OCT angiography (optical coherence angiography), which is an innovative, pain-free and non-invasive method for making the blood flow visible. It is only possible to make blood flow visible without using contrasting agents in two locations in the body – the eye and in the nail fold, which is the junction between the nail bed and the finger. Ophthalmologists at Universitätsklinikum Erlangen have been able to offer this examination method to patients after a Covid-19 infection as part of a clinical study since 2020. Initial evaluations show that the flow of blood in the eye is significantly limited for several months after recovery, even if patients are not suffering from any impairments to their vision. The clinical study with patients after a Covid-19 infection continues. Together with scientists at the Max Planck Center for Physics and Medicine in Erlangen and the team led by Dr. Wallukat, investigations are now being carried out for the mechanisms that can lead to limited blood flow and that could explain the mode of action that led to the successful treatment.
Link to abstract about the study: https://www.frontiersin.org/articles/10.3389/fmed.2021.676554/abstract
Further information:
Dr. Dr. Bettina Hohberger
Phone: +49 9131 85 33001