Stem cells as a window to the brain
FAU researchers clarify mechanism behind spastic paraplegia
A team of FAU researchers has taken some important steps towards finding treatments for a specific form of hereditary spastic paraplegia, a group of neurodegenerative diseases for which there is currently no known cure. In a human cell culture system the researchers were able to treat neural progenitor cells taken from patients with a substance that had a positive effect on the cells. They hope that in the long-term their findings could lead to the development of a new treatment.
Gene mutation triggers paraplegia
Hereditary spastic paraplegia (HSP) is caused by a mutation of the gene SPG11. A specific characteristic of this gene mutation is that, in addition to HSP, it also leads to cognitive impairment. There is currently no cure for HSP, which begins during childhood and adolescence, reaching an advanced stage by early adulthood at the latest. Children with HSP reach important milestones in their physical and mental development later than their healthy peers. Cognitive problems when completing complex everyday tasks become apparent during early adulthood. It is not until after this that patients begin to experience problems walking due to weakness of the legs, which increases as the disease progresses and results in needing to use a wheelchair and requiring assistance from others.
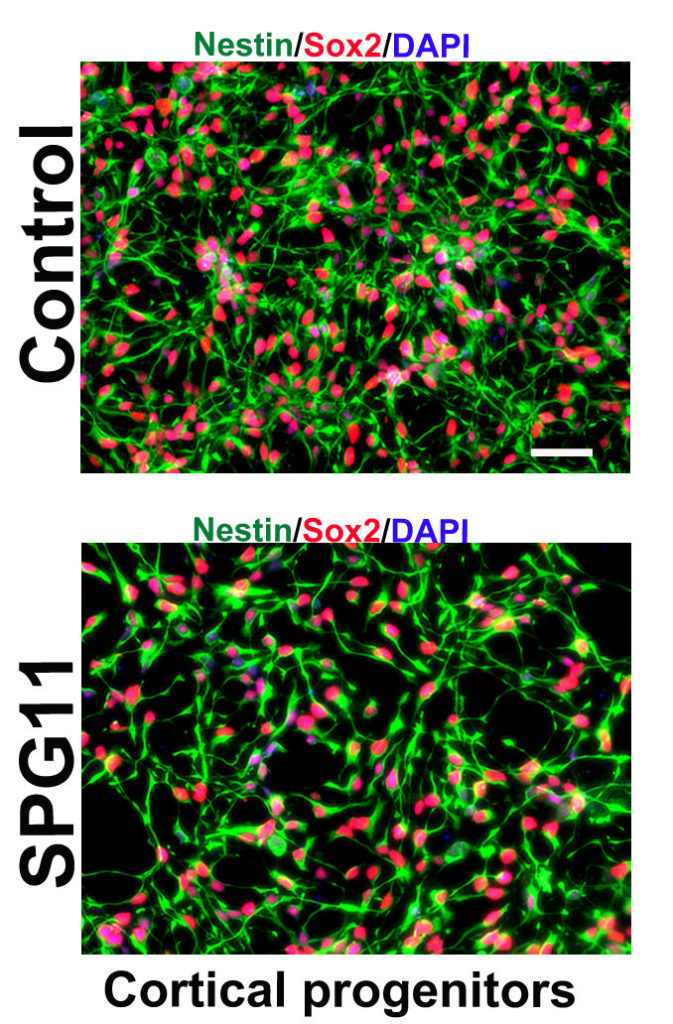
An FAU research group has now taken some important steps towards finding a cure for the disease with the help of funding from Tom-Wahlig Stiftung, the world’s first HSP foundation. The patients who took part in the group’s study were looked after by Prof. J. Winkler and PD Dr. Z. Kohl from the Department of Molecular Neurology. The researchers took small skin samples from the upper arms of HSP patients and healthy individuals. They then transformed the cells from the samples into pluripotent stem cells – cells that can change into any other type of cell. In this study the stem cells were transformed into patient-specific neural progenitor cells. The researchers from Junior Research Group 3 at the Interdisciplinary Centre for Clinical Research (IZKF) at Universitätsklinikum Erlangen were able to demonstrate that the neural progenitor cells from the HSP patients divided less frequently than health cells.
Biochips and potent substances
‘We were able to attribute the fact that healthy cells divide more frequently than diseased ones to disruptions during cell development and to identify the associated signalling pathway,’ explains Dr. Himanshu Mishra, who studied this subject in his doctoral research. The researchers made their discovery using gene chip analysis carried out by FAU’s Institute of Human Genetics. This is a highly complex process that allows several thousand gene sequences to be tested at the same time and compared with one another.
In the next stages of the research project the group, led by Prof. B. Winner, was able to correct the anomalies associated with the disease. This was achieved with a highly potent substance called tideglusib that is currently being tested as a possible treatment for Alzheimer’s disease. It works on the molecular level by suppressing chemical processes that are thought to play an important role in cognitive processes. Unfortunately, it is not yet possible for the FAU researcher’s approach to be used in therapy. ‘However, we hope that by establishing models of disease based on human nerve cells our research will enable new substances to be discovered and tested, and that we will be able to help patients suffering from the disease,’ says Prof. Dr. Beate Winner, head of IZKF Junior Research Group 3 and professor of stem cell models of rare neural diseases at the Institute of Human Genetics.
Further information:
Prof. Dr. Beate Winner
Phone: +49 9131 8539301
beate.winner@fau.de
